Precision Cardiovascular Monitoring with Non-Invasive Hemodynamic Assessment
Introduction
Accurate, real-time assessment of hemodynamic parameters such as blood flow and tissue perfusion is critical for diagnosing and managing cardiovascular diseases. Traditional methods for measuring these parameters, such as catheterization or imaging techniques, can be invasive, time-consuming, and uncomfortable for patients. Our patented technology provides a groundbreaking non-invasive solution for assessing hemodynamics using a coherent light source, allowing for real-time, accurate measurements of blood flow and tissue health without the need for invasive procedures. This innovation stands to transform how healthcare providers monitor and diagnose cardiovascular health.
The Need for Non-Invasive Cardiovascular Monitoring
Cardiovascular diseases are the leading cause of death globally, making early detection and monitoring of vital hemodynamic parameters essential in managing patient outcomes. Traditional diagnostic methods, such as angiography, ultrasound, and invasive pressure monitoring, often come with significant discomfort, risks, and limitations in accessibility. These methods can also be impractical for continuous monitoring, which is needed in critical care settings or for patients with chronic conditions. The healthcare industry requires a less invasive, more accessible way to monitor cardiovascular health in real-time.
For patients, non-invasive monitoring systems would offer a more comfortable, accessible, and continuous method of tracking their cardiovascular health, improving patient adherence and quality of care.
A Breakthrough in Non-Invasive Hemodynamic Assessment
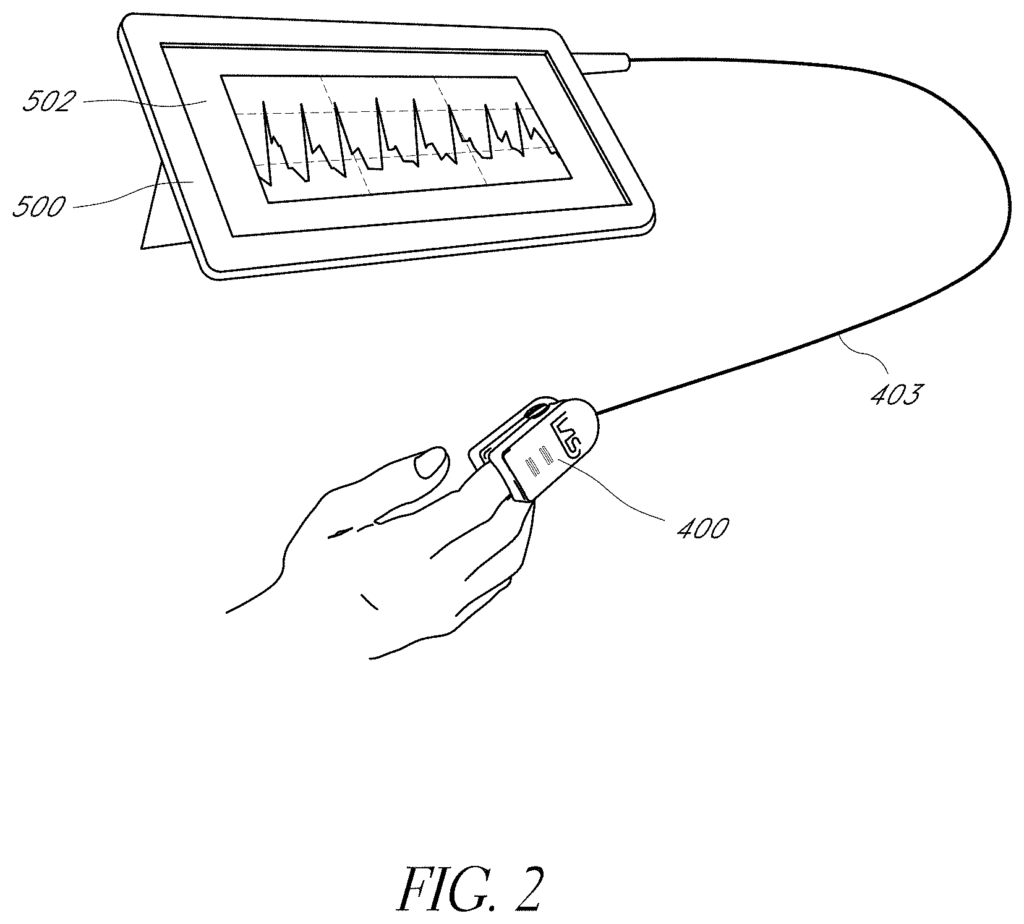
Our patented technology uses a coherent light source to interrogate biological tissue, enabling non-invasive assessment of hemodynamic parameters. By detecting changes in light patterns as they pass through tissues, the system provides real-time data on blood flow, tissue perfusion, and vascular health. This makes it ideal for a range of applications, from monitoring patients in critical care to offering continuous assessments for those with chronic cardiovascular conditions.
The device’s non-invasive nature means it can be deployed in both clinical and home settings, enhancing telemedicine capabilities and enabling remote patient monitoring. With its real-time feedback, this technology is particularly useful for early detection of issues such as ischemia or vascular dysfunction, helping healthcare providers make timely and informed decisions.
Key Benefits
- Non-Invasive Monitoring: Eliminates the need for invasive procedures, offering a more patient-friendly diagnostic experience.
- Real-Time Data: Provides immediate insights into hemodynamic parameters, allowing for quicker clinical decisions.
- Versatile Applications: Useful for both in-hospital and remote monitoring, expanding its utility in telemedicine and chronic care management.
- Enhanced Cardiovascular Care: Improves the ability to monitor and manage cardiovascular diseases more effectively.
A New Standard for Cardiovascular Diagnostics
Licensing this technology offers medical device manufacturers and healthcare providers an innovative tool for non-invasive, real-time cardiovascular monitoring. With the potential to improve patient outcomes and streamline diagnostics, this technology is poised to become a key asset in modern cardiovascular care.
- Abstract
- Claims
What is claimed is:
1. A system for determining one or more physiological parameters in a subject, the system comprising:
c. a processor comprising a program and a memory, wherein the processor is operably coupled to the photo-sensitive detector and configured to receive and store in memory the raw signal from the photo-sensitive detector generated over a period of time, and wherein the processor is further configured to generate a first waveform and a second, physiologically distinct waveform from the first waveform based on the raw signal;
ii. calculate the first waveform from the contrast metrics and the second waveform from the intensity metrics;
10. A method for determining one or more physiological parameters from particles in pulsatile motion within a physiological system, the method comprising:
Share
Title
Non-invasive hemodynamic assessment via interrogation of biological tissue using a coherent light source
Inventor(s)
Tyler Bywaters Rice, Michael Ghijsen, Bruce J. Tromberg, Bruce Yee Yang, Sean Michael White
Assignee(s)
University of California, Covidien LP
Patent #
10813597
Patent Date
October 27, 2020