Advanced Monitoring for Pulmonary Artery Pressure in Critical Care
Introduction
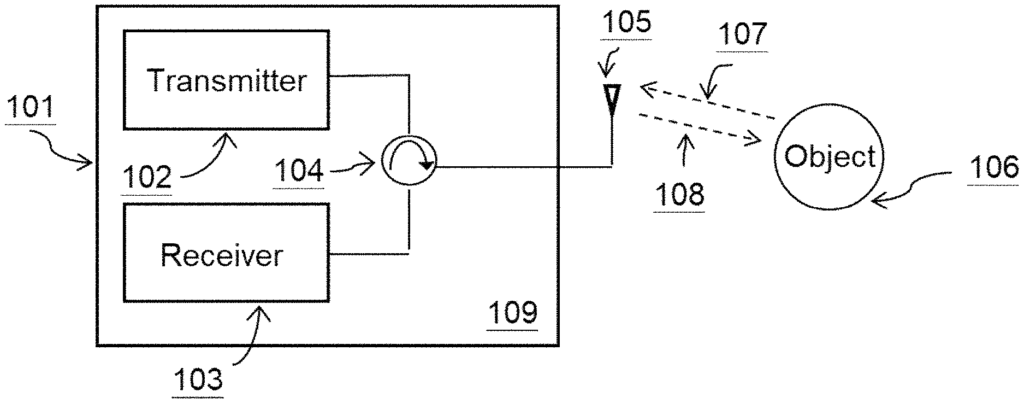
Chronic heart failure and pulmonary artery hypertension are conditions that require meticulous monitoring to prevent sudden complications. Monitoring pulmonary artery pressure (PAP) provides crucial insights into a patient’s cardiovascular and pulmonary status, helping clinicians detect early signs of deterioration and adjust treatment plans accordingly. Our patented pulmonary artery pressure change monitor offers a cutting-edge solution to this ongoing need, providing real-time monitoring that enables early intervention and improved patient outcomes.
Current Limitations in Monitoring Pulmonary Artery Pressure
Traditional methods for monitoring pulmonary artery pressure often involve invasive procedures or intermittent assessments, which limit their usefulness in real-time management of conditions such as heart failure or pulmonary hypertension. These approaches may not provide the continuous data necessary to detect subtle changes in a patient’s condition, leading to delayed interventions and potentially worsening outcomes. For patients who are prone to sudden pulmonary or cardiac complications, real-time monitoring is critical for preventing acute events like heart failure exacerbation or pulmonary edema.
The healthcare industry is moving toward more personalized and real-time approaches to care, where continuous monitoring can provide early warnings and allow for immediate medical adjustments, thereby reducing hospital readmissions and improving quality of life.
A Game-Changing Approach to Pressure Monitoring
Our pulmonary artery pressure change monitor is designed to provide real-time, non-invasive or minimally invasive monitoring of pulmonary artery pressure changes, making it easier to track a patient’s condition over time. By detecting subtle fluctuations in pressure, this system enables healthcare providers to proactively adjust treatments, reduce the risk of complications, and offer more personalized care. The monitor is ideal for use in both hospital settings and at home for remote patient monitoring, making it versatile for a wide range of clinical applications.
This advanced system allows physicians to have continuous insight into a patient’s cardiovascular status, offering real-time data that can inform treatment decisions and reduce the need for more invasive procedures. By integrating this technology into routine care, healthcare providers can offer better management of chronic conditions, improve patient outcomes, and reduce costs related to emergency interventions.
Key Benefits
- Real-Time Monitoring: Provides continuous data on pulmonary artery pressure, allowing for immediate intervention when necessary.
- Non-Invasive or Minimally Invasive: Reduces the need for traditional invasive monitoring methods.
- Improved Patient Management: Enables personalized care plans for chronic conditions like heart failure and pulmonary hypertension.
- Versatile Use: Suitable for both in-hospital care and remote monitoring at home, expanding its applicability in modern healthcare.
Advancing Cardiovascular Care with Real-Time Insights
Licensing this pulmonary artery pressure monitor technology offers medical device companies and healthcare providers an essential tool for advancing patient care in cardiology and pulmonology. With its ability to provide continuous, real-time data, this technology is critical for improving patient management and outcomes in chronic cardiovascular and pulmonary conditions.
- Abstract
- Claims
What is claimed is:
1. A method of detecting a heart failure condition in a heart in a body of a subject, comprising:
Share
Title
Pulmonary artery pressure change monitor
Inventor(s)
Xiaomeng Gao, Xiaonan JIANG, Xiaoguang Liu, Dennis Matthews, Saul Schaefer
Assignee(s)
University of California
Patent #
11647978
Patent Date
May 16, 2023